

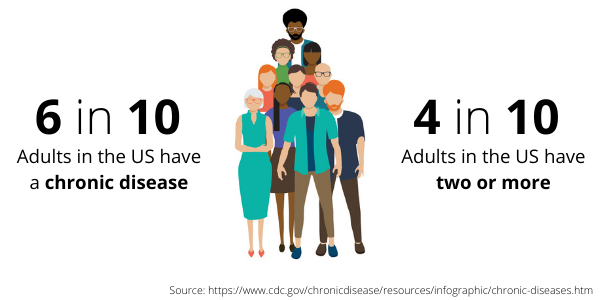
A comorbidity can be defined as the presence of two or more diseases or medical conditions in a patient. Hypertension, high cholesterol, obesity and chronic obstructive pulmonary disorder (COPD) are just a few of the most common coexisting health conditions around the world. These comorbidities, combined with other factors such as age, compound the risk of poor health outcomes.
As we’ve covered previously, morbidity patterns are the strongest predictor of resource use, so if providers want to reduce costs and improve care, they have to address the highest-need patient groups. Fortunately, the ACG System excels at helping users understand comorbidities in their populations, giving them vital information to drive effective care solutions.
So how does it work? The ACG System has an array of specific analytical markers to help guide users to the most high-risk patient group to proactively ensure they get access to the care they need.
For example, let’s say a health system wants to identify patients with metabolic syndrome – this includes a combination of hypertension, dyslipidemia and obesity. When present, these conditions increase the risk of cardiovascular disease and diabetes, both of which can be costly and intensive for patients and providers alike. The ACG System easily allows for users to build out their own custom list of patients with analytical markers, such as probability of hospitalization in the next 6 months, total costs, risk scores and Emergency Department visits—they can even identify which of those visits may be preventable. In addition, a review of this group’s medications may also reveal some patients who may not be in control of, or not adhering to, their hypertension or medication regimen or recommended lifestyle changes. This deep-level understanding identifies specific issues for health care providers to address, and concrete actions they can take to reduce costs and improve care.
Ultimately, understanding common comorbidities and the impact on medical costs is crucial so that health care organizations can meet new value-based standards and increase the quality of life for the patients they serve.
Learn more about how the ACG System helps to identify and understand comorbidities by reading these related blog posts:
Addressing multimorbidity is critical to an effective population health strategy
Quick Win #3: Effectively manage multimorbidity
Or download the Multimorbidity Infographic.
Follow Us