

A team from the Johns Hopkins Center for Population Health Information Technology has published a new paper in the Journal of Population Health Management called “Integrating Social and Behavioral Determinants of Health into Population Health Analytics: A Conceptual Framework and Suggested Road Map”, says Jonathan P. Weiner DrPH, Professor of Health Policy & Management and of Health Informatics, CPHIT Director, ACG Co-Developer and Director of the ACG R&D Team at Baltimore’s Johns Hopkins Bloomberg School of Public Health.
Citing “growing recognition that social and behavioral risk factors impact population health outcomes,” the article reports on a study that “reviews existing literature and proposes a conceptual framework for the integration of social and behavioral data into population health analytics platforms.” It describes several use cases for integrated platforms: at the patient, health system and community levels. It also aligns the use cases with the types of prevention identified by the Centers for Disease Control & Prevention and “explores available and potential future sources of social and behavioral domains data.”
Here are excerpts from the article (as featured in the May 2019 edition of Care Analytics News):
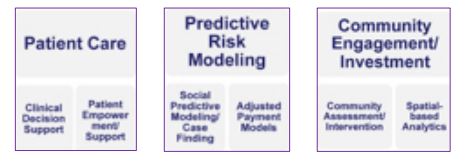
According to the researchers, Use Case 1 is patient care; applications include clinical decision support and patient empowerment, because “increased integration of SDOH information could allow clinicians to tailor and modulate care as needed –a clinician’s knowledge of a diabetic patient’s social and behavioral risk factors, such as having food insecurity, for example.” SDOH-centric decision support also could “provide tools tailored to the needs of patients, empowering self navigation of available social services.”
Use Case 2 is predictive risk modeling. Most models now are “based on claims and clinical data from EHRs and, because of a lack of data, usually do not incorporate social and behavioral risk factors beyond simple demographics such as age, sex and race,” the report notes. But “a significant and growing body of literature” suggests that incorporating those factors “might improve predictive power for both adult and pediatric populations;” there also are “opportunities to integrate those factors into adjusted payment models.”
The applications of Use Case 3 include “community assessment, community-level intervention and small-area analysis,” the paper explains. Integration of community-level social and behavioral risk factors – or, “community vital signs” — into population management tools “helps integrated health systems address them with interventions tailored to community
needs and priorities.”
 Those activities “would correspond to the CDC’s third bucket of prevention: total population or community-wide interventions,” the paper adds, “which include efforts affecting an entire population, usually within a specific geographic area.” The article lays out these challenges:
Those activities “would correspond to the CDC’s third bucket of prevention: total population or community-wide interventions,” the paper adds, “which include efforts affecting an entire population, usually within a specific geographic area.” The article lays out these challenges:
The conversation around SDOH has “reached a crescendo,” the article says. “Clinicians and plans must, in the near term, find ways to more effectively introduce social and behavioral factors into the medical care process.”
The timing is good. Health departments everywhere “are in the midst of their own transformative paradigm shift known as ‘Public Health 3.0’,” the researchers add. Its “hallmark,” they say, “is the use of advanced data systems in support of crosssector initiatives for integrating medical, SDOH and public health interventions.” In fact, despite the obstacles, the researchers assert, “there is little question that a social and behavioral determinant-enabled, population-centric analytics platform will be necessary.”
Care Analytics News talked to three of the paper’s authors — Zachary Predmore, Elham Hatef MD MPH and Jonathan Weiner DrPH — about the terms of meaningful integration and what’s going to be required in the future in addition to today’s technical and data sciences skill sets.
Predmore, Hatef & Weiner: We believe this framework could be widely used to help guide the integration of SDOH data of all types. Various important parties have demonstrated interest in trying to integrate data from multiple sources, but there has been no one common framework that covers most applications. We believe that our framework comes close to achieving this. We hope those who work in this field will agree and will build and improve on what we have done.
About the scope question: Individual organizations involved in this space may not have a big enough footprint to deal with all facets we lay out. Rather, they may use pieces of our framework that are relevant to their goals. For example, a population-based primary care practice may be more interested in Use Case 1, ‘patient care,’ while a public health agency may be more interested in Use Case 3, ‘community engagement and investment.’
Meaningful integration will not be an all-or-nothing state. As many of the papers we cite in our literature review indicate, at this time, stakeholders are integrating sub-sets of variables into their population health analytics programs. We expect to see more integration of multiple data sources as data availability and technology improve in the future.
PH&W: We are currently seeing a mixture of public and private leadership on these issues. To date, federal funding is playing a key role in funding R&D to address some of the unresolved questions (e.g., the validity of using neighborhood-level data for estimating the risk of individuals), but private entities will be essential for the development of solutions to these problems. One challenge that we have seen with some of the private sector advances is the lack of transparency and openness for scientific validation. We hope that might change in the future if the field is really to take off nationally.
PH&W: An answer to your question probably involves a balance of two countervailing factors. First, healthcare, social and economic environments, as well as data systems and sources, will tend to be similar across comparable types of US jurisdictions (e.g., inner city or rural areas). In addition, the challenges faced by comparable organizations (e.g., hospitals, PCMHs, governments, health plans or public health agencies) will
likewise be similar. On the other hand, as is often said about politics, “all SDOH issues are local;” that is, many of the factors facing certain communities and individuals regarding their sociobehavioral challenges and contexts may not transfer well from region to region.
PH&W: As some of us — and other Johns Hopkins faculty colleagues — discussed with you in previous editions of your newsletter after publishing journal articles on NLP and ML, neither of these data science techniques are panaceas. They represent tools that can, at times, be used to advantage as part of a well-thought-out analytic approach. But, yes, NLP in particular will be key to advances in the near future, as a large amount of SDOH information is now locked in the “free text” of EHRs and social service agency written records. As noted in the past, these techniques are not alternatives for real-world paradigms and well-thoughtout use cases, so the conceptual frameworks such as the one featured in our article will still be key.
PH&W: Some of the learning and growth challenges associated with SDOH analytics are similar to those faced in other more general population and clinical analytics domains. But some learning-curve challenges faced by organizations and staff will be a bit different. In addition to the normal technical and data sciences skill sets, an understanding of the range of social and non-medical contexts and data sources will also be needed. It will be good for those developing SDOH analytics platforms to find ways to break down existing silos across service provision sectors to expedite this learning.
PH&W: We encourage readers conducting work in this area to consider using the framework we have developed as they plan and implement their analytic activities. We look forward to hearing from them as to whether it is helpful and how it might be improved upon. Also, the literature review we present in this paper should be useful to those seeking to better understand the current state of knowledge on linkage between SDOH factors and medical outcomes. Speaking of advancing knowledge, our group at CPHIT has a wide array of SDOH R&D projects under way. For example, working with colleagues at the VA, we recently published a study where we linked millions of EHR records across the VA’s national PCMH program to assess the impact of SDOH factors on hospitalizations. We also have projects ongoing where we are linking SDOH information from both geo-level and individual-level databases into our more clinically oriented Johns Hopkins ACG predictive modeling platform.
Click here to read the paper “Integrating Social and Behavioral Determinants of Health into Population Health Analytics: A Conceptual Framework and Suggested Road Map”.